Many have asked so I thought it might be helpful to just post it on here - the WHO, WHAT, WHEN, WHERE & WHY of it all...
WHAT: Spine surgery #7: (1) Repair CSF leak, (2) Exploration of spinal fusion
WHEN: Tuesday, July 23rd, 2013 (arrive at hospital 6am, surgery starts 8am)
WHERE: Cooper University Hospital - 1 Cooper Plaza, Camden NJ - 08103
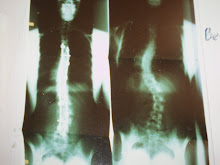
WHY: This is a tricky one but I'll try to summarize simply and concisely. I have a cerebrospinal fluid leak (CSF) which stems from the leak discovered in my most recent spinal reconstruction last November 2012. At that point, it was 'plugged' with the screw at T12 (the vertebra I fractured at 6 wks post-op in March 2012) in a washout surgery just 4 days after the larger one in November where they extended my fusion up to T2 and down to S1 into my pelvis (w/ pelvic anchors). In Feb 2013, I began experiencing severe, debilitating headaches - I tried everything (sinus surgery, new glasses) to try and eliminate the headaches but nothing worked. We moved from NJ to PA at the end of April and 4 weeks later I was in the ER, admitted with severe headaches after a brain MRI showed a significant CSF leak. I spent a week in the hospital and then spent the next 6 weeks seeking out 2nd, 3rd, 4th opinions. And they all said the same thing: surgery to fix the leak. I am not a candidate for the lesser and much less invasive "blood patch" due to the sheer volume of bone graft and fusion bone not to mention hardware in my spine.
DETAILS of SURGERY: They will explore the fusion in both the thoracic and lumbar areas in hopes of locating and fixing the CSF leak. There is no guarantee that they'll even be able to locate it despite having evidence that one most likely exists at the level of T12 where the previous leak was. They have no idea about the length of surgery (stating "it could take 4 hours or 14, we simply have no way of knowing until we get in there and see what we're up against"), length of stay in the hospital, length of recovery or even what to expect pain-wise post-operatively. I was in the ICU for an unusually long time last surgery, 3 days. Typically one spends about 24 hrs in there and then moves to a regular room. Since nothing is "typical" or "regular" with me, the hospital has already prepared for the atypical, unusual surprises that most likely will come their way regarding my post-op care and recovery.
My Dad accompanied me this afternoon as we went to Cooper University Hospital to meet with the ICU Nursing and Management team. We met with the Clinical Director (MaryJo Cimino, one of Cooper's finest - she is the most wonderful, knowledgeable and experienced critical care nurses I have ever had the pleasure of meeting or knowing), the Assistant Clinical Director (Suzanne Gould, another one of Cooper's finest nurses), Maresa Class (Patient Representative and advocate for any and everything patient-related). We had a good discussion and they all helped to put some of my fears at ease...they can't guarantee anything, but they can guarantee that all the ICU and Neuro nurses who work with me will be fully informed and kept up-to-date on my medical issues and circumstances. That's all I can ask for. I know I will be in very competent, skilled hands with MaryJo and her team as well as my amazing and highly skilled neurosurgeon, Dr. Steven Yocom and orthopedic surgeon, Dr. David Clements.
Hi this is really a great sharing from this source i must say you have done a great work this will give lots of inspiration to many patient. Again Nice Sharing.
ReplyDeleteISO 2338
ISO 2341
DIN 1444
Thank you "Anonymous" (7/20/13), for your comment. It means alot to mean to think that some people may find my blog inspiring and helpful or informative. That means I am accomplishing my, which is to reach people who may not know alot about scoliosis OR just the opposite, to reach people who know quite a bit about scoliosis - and give them a first-hand, honest account of what it's really like to be living with this condition, through the good, the bad and the ugly.
Delete